Claims Adjudication
Overview of Claims Adjudication
On this page
What is Claims Adjudication?
MOH started adjudicating MediShield Life claims against prevailing MOH guidelines and requirements in October 2022. Adjudication happens after the claim has been settled, thus preserving the current claim submission process.
Claims Adjudication augments the current Table of Surgical Procedures (TOSP) surveillance audits conducted by MOHH's Group Internal Audit to encourage the provision of medically necessary treatments and prudent use of healthcare resources.
How are cases selected for Claims Adjudication?
Claims for adjudication are selected from two main sources:
Cases that have been whistle-blown by patients, doctors, and insurers, and
Cases where claims have been found to have deviated from peer norms, speciality-specific Claims Rules and general financial claims rules and guidance issued by MOH e.g. Table of Surgical Procedures (codes for claiming fees for surgery), MediSave booklet, Agency for Care Effectiveness guidance
What are the common types of Inappropriate Claims
Common categories of inappropriate claims are as follows:
Inappropriate use of TOSP codes, such as
using proxy TOSP code(s) that do not accurately describe the procedure performed
submitting more than one TOSP code where a single TOSP code adequately describes the episode of surgery/procedure carried out (e.g. submitting multiple codes for doing Whipple’s procedure instead of the code describing Whipple)
performing each component procedure in a separate episode of surgery, for procedures that could otherwise be performed under a single TOSP code and/or episode of surgery/procedure
submitting TOSP codes for procedures which were not performed (This can constitute fraud, which can be prosecuted as a criminal offence)
Over-servicing, such as
unnecessary tests performed during an episode of admission
surgical treatment done before trial of conservative treatment (e.g. gastroscopy done on patient with 1st episode of gastritis before trial of antacids)
unnecessary admissions for procedures that are commonly done in day surgery and attempt to claim health screening tests from insurance (usually not claimable)
Claims for procedures excluded by MediShield Life, including,
cosmetic procedures and health screening under disguise of diagnostic procedures/treatment. This can constitute fraud, which can be prosecuted as a criminal offence
What is the process for Claims Adjudication?
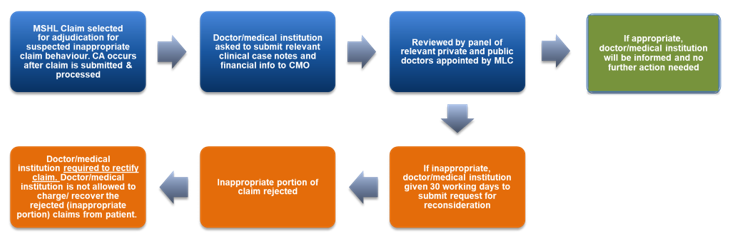
Cases are adjudicated by an independent Panel of 3-6 doctors appointed by the MediShield Life Council (MLC). The doctors are of the relevant speciality for the case in question, from both private and public sectors
If a MediShield Life claim is selected for adjudication, the medical institution and doctor concerned will be notified in writing and be required to submit relevant clinical case notes and justifications to explain any deviation from MediShield Life claim requirements to the Panel
Doctors would subsequently be informed of the outcome after the Panel has completed its assessment. The various types of outcomes are as follows:
If the Panel deems the claim to be appropriate for the patient, no change is required for the claim (i.e. MediShield Life and MediSave payout remains)
If the Panel deems the claim to be inappropriate, the medical practitioner and his / her patient may, within 30 working days of receiving the Panel’s assessment, submit new evidence to the Panel for reconsideration. However, if the Panel still concludes the claim to be inappropriate, the adjudication decision is final. The medical institution and the doctor will be asked to re-file the claim to rectify the inappropriate portion of the claim so that the MediShield Life and MediSave payouts could be adjusted and appropriately reflected. They should not shift inappropriate charges to other parts of the bill nor recover from patients
Please click here for "5 Facts on Claims Adjudication" infographic [PDF 989 KB]
Factors Considered in Determining Appropriateness of a Treatment Under a MediShield Life Claim*
In assessing the appropriateness of a treatment under the MediShield Life Claim, the Panel will consider the following, whether the claim is:
Aligned to the Singapore Medical Council’s Ethical Code and Ethical Guidelines
In accordance with current generally accepted standards of medical practice (peer reviewed journals, MOH Guidelines, ACE guidance, consensus statements, peer concurrence etc.)
Clinically appropriate in terms of type, frequency, extent, site, and duration, and considered effective for the insured person's illness, injury, or disease
Not primarily for the convenience of the insured person, medical practitioners or medical in situations where treatment is able to be reasonably rendered in an outpatient setting
Not of an investigational or research nature/unapproved by regulatory authorities
Not preventive, screening or a health or aesthetic enhancement and
Aligned with prevailing guidelines published by MOH and its appointed agencies, where relevant, including but not limited to MediShield Life Claims Rules, TOSP Booklet, Manual on MediSave/MediShield Life claims, Terms and Conditions for Approval under MediSave/MediShield Life schemes, MOH Finance Circulars related to MediShield Life/MediSave claims and ACE’s guidance, as far as such guidelines relate to the medical appropriateness of the treatment
*Above list is not exhaustive
Enforcement against non-compliant providers
MOH will take action against providers with repeated non compliances to deter inappropriate claim behaviours. These include warnings and mandatory training to refresh the doctor on rules governing MediShield Life claims:
From 1 Apr 2023, providers with repeated non-compliances can have their status as approved Medical Practitioner under the MediShield Life and MediSave be suspended or revoked. This would mean that the doctor will not be able to submit any claims for MediShield Life, MediSave and Integrated Shield Plan (IP) Insurance.
Doctors will be referred to the Singapore Medical Council (SMC) if their practices were assessed to potentially contravene SMC Ethical Code and Guidelines
Lastly, where an individual has made a false declaration, omits information, or provides information which is false or misleading in a material that results in a claim being overpaid, they can be prosecuted under Section 19 of the MediShield Life Act. MOH may also refer cases of potential fraud to the police for criminal investigation and prosecution