Allied Health Training Pathways
Revamping AHP Training
On this page
The need to relook at Allied Health Training
Allied Health Professionals (AHPs) are essential members of the healthcare team and have the potential to drive efforts to shape future care delivery. Traditionally, AHPs are trained within their distinct profession. As Singapore’s population ages and care needs are becoming more common in the community and social settings, there is a need for AHPs to be more versatile, working more collaboratively across professions to deliver care holistically.
Understanding the approach
Modular training is increasingly common in the healthcare sector and enables healthcare professionals to acquire new skills to broaden and deepen their professional expertise more easily and readily. Some modular training takes the form of workplace-based training, where learning is integrated at workplaces.
The new Allied Health training approach is centred on building a training system that provides flexibility for AHPs to acquire additional competencies without compromising professional competencies, standards of care, and regulation. We fully recognise the unique expertise of each profession, and the required qualifications for entry into the respective professions will remain. They can gain additional skills based on aspirations or setting requirements.
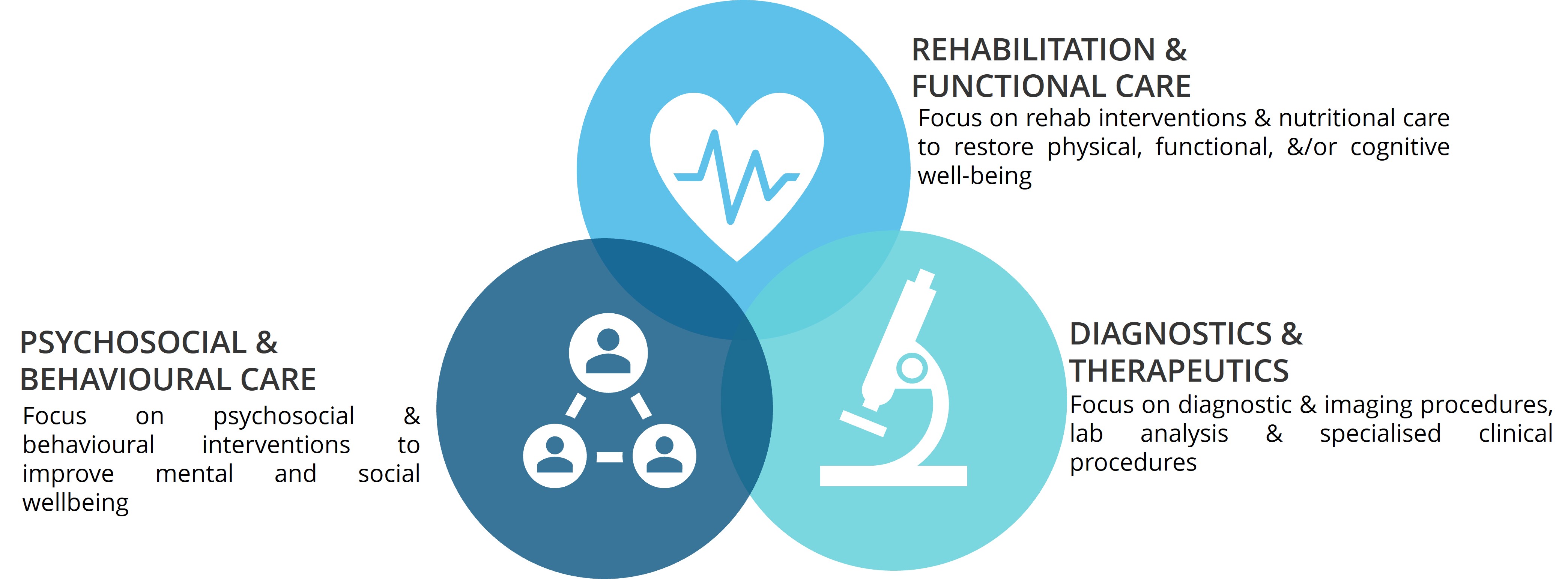
Professions that are adjacent in practice scope were grouped together into 3 key domains (see diagram below) to better enable identification of common core competencies and additional competencies beyond the profession’s typical scope that can be attained to improve breadth of practice at the basic level.
Some current examples of the training for common competencies include:
(i) Inter-professional Skills Based Behavioural Health for Health Professionals (for occupational therapists and physiotherapists) delivered by the Singapore Institute of Technology (“SIT”);
(ii) Inter-professional Workshop on Cognitive Rehabilitation for Persons with Cognitive-Perceptual Dysfunction (for occupational therapists, nurse clinicians, and other AHPs) delivered by SIT, and
(iii) National Prescribing Practitioner Programme (for advanced practice nurses and senior pharmacists) by the National University of Singapore.
These competencies can be developed through enhancing undergraduate curriculum or adopting a modular and stackable approach for continuous professional education.
Frequently Asked Questions
1. Does such categorisation limit the scope of practice or the learning opportunities for my profession which straddles between 2 domains?
No. The domains are meant to describe broad groupings based on adjacency in professional scope and service delivery, intended to help identify shared competencies for professions to work together.
AHPs who impact care in more than one domain currently may continue to do so. The current scope of practice, core expertise and professional identity of each profession remain unchanged with the categorisation.
2. Why is there a need for shared competencies across AHPs, and how would it work?
Shared competencies across AHPs create a “common language” among AHPs to complement each other’s expertise and facilitate collaboration, contributing towards holistic care in a more seamless way and enhances the overall effectiveness of the healthcare team.
This aims to allow AHPs to better complement one another under a team-based shared-care model, while practising within clearly defined limits. It benefits patients, with an increasing number of seniors with multiple and complex chronic medical conditions. This is about enhancing collaboration, not merging or replacing the professions.
3. How will the “modular, stackable, workplace training” modules work in practice? Will AHPs be able to accumulate credits towards formal qualifications?
Modular training enables learners to accumulate credits towards formal qualifications. This would mean being able to acquire and apply new competencies relevant for their career growth and service needs more efficiently.
4. How will standards continue to be maintained with the new approach?
As we implement this approach, the pathway will be built on clearly defined learning outcomes to ensure consistency in training standards.
MOH will continue to work closely with educational institutions, professional associations, healthcare professionals, and relevant stakeholders to shape the future of Allied Health while enhancing care for clients and patients and upholding professional standards.
5. I am currently a year 1 undergraduate pursuing an AHP degree. Will the change towards modular, stackable learning or the introduction of shared competencies affect my current studies?
There will be no change to the existing curriculum and regulation for existing students.
MOH is in discussion with Institutes of Higher Learning (IHLs) and we expect changes to be rolled out for relevant programmes, starting with students who begin their studies from AY2027 onwards.